COPY
Current Status: Active PolicyStat ID: 6960786
Origination: 07/2007
Effective: 01/2013
Last Approved: 04/2021
Last Revised: 04/2021
Next Review: 04/2023
Owner: Shawn McCardell:
Director PFS
Area: Finance
Standards & Regulations:
References:
Self Pay Collections, FN 101
1. FHH/FHMG expects patients to pay for services at the time service is provided or within thirty (30) days of
the first billing statement for services not covered by insurance or financial assistance.
2. FHH/FHMG must take effective action to maintain timely accounts receivable turnover and ensure that
the value of accounts receivable is accurately stated. To do this, patient accounts will be aged and written
off as bad debts or charity and may be outsourced to collection agencies for further follow-up.
3. Emergency services will be provided to all patients regardless of ability to pay. Scheduled services will be
provided after appropriate financial arrangements are confirmed by FHH/FHMG. Deposits may be
required prior to scheduling services. Failure to pay required deposits may result in the rescheduling of
non-emergent services.
4. Financial assistance may be available for patients based on financial need, including as a result of a
medical hardship, as defined in the FHH/FHMG Financial Assistance Policy.
a. It is the patient's responsibility to provide accurate information regarding address, employment and
health insurance in order to determine eligibility for financial assistance.
This policy applies to all patient accounts identified as self-pay or with a remaining patient responsibility after
insurance and/or financial assistance for services provided by Frederick Health Hospital ("FHH") or Frederick
Health Medical Group ("FHMG"). FHH and FHMG are collectively referred to in this policy as FHH/FHMG.
This policy applies to any employee of FHH/FHMG who performs collection activity in the Patient Financial
Services ("PFS") Department. This policy is intended as a guideline to assist in the delivery of patient care or
management of hospital services. It is not intended to replace professional judgment in patient care or
administrative matters.
PURPOSE:
The purpose of this policy is to establish a policy and procedure for initiating collection actions and the write-off
of accounts receivable as well as the subsequent placement of the receivables with outside agencies or
attorneys for collection. This policy documents a consistent practice for collecting amounts due from patients,
regardless of insurance coverage, and the procedures necessary to record write-offs taken.
This policy is intended to comply with Section 501(r) of the Internal Revenue Code and applicable Maryland
law. It has been adopted by the Board of Directors of FHH and Frederick Health, Inc. and shall be reviewed
and approved by such Boards every two years.
POLICY:
Self Pay Collections, FN 101. Retrieved 04/2021. Official copy at http://fmh.policystat.com/policy/6960786/. Copyright ©
2021 Frederick Health
Page 1 of 5
COPY
5. FHH/FHMG complies with all state and federal law and performs its credit and collection functions in a
dignified and respectful manner.
6. FHH/FHMG does not discriminate on the basis of race, sex, age, color, national origin, creed, marital
status, sexual orientation, gender identity, disability, or ability to pay.
7. FHH/FHMG may use external collection agencies for extended business office, legal and/or collection
activity to assist with collecting on patient accounts. FHH/FHMG will provide active oversight of any
collection agency that collects debts on their behalf, and such agencies shall be required to abide by this
policy and applicable provisions of the Financial Assistance Policy.
1. Cash Collections
a. Payment for identified co-payments and deductibles will be requested prior to or at the time of service. In
the case of emergency services, no payment shall be requested until after a patient has received a
medical screening exam and any necessary stabilizing treatment.
i. FHH/FHMG accepts cash, checks and credit cards to settle outstanding accounts.
ii. Medically necessary care will not be deferred or denied due to an outstanding balance for previously
provided care.
b. Subject to FHH/FHMG approval and as described in the Financial Assistance Policy, payment
arrangements may be made for patients who have difficulty paying in full.
i. Where appropriate, payment arrangements may be set up to resolve open balances within a
reasonable timeframe.
ii. Payment arrangements that remain current will not be forwarded to bad debt collections.
c. If a patient's check is returned from the bank for not-sufficient funds, the check may be deposited again or
the amount of the check will be added back onto the account as an unpaid balance. FHH/FHMG may
charge a reasonable fee for all returned checks that will become part of the patient's financial
responsibility
d. There may be scenarios that occur during the collection process outlined in this policy that may result in
placing a hold on collection efforts (called an "administrative hold") until additional information is provided.
All accounts on administrative hold will be compiled into a report by threshold levels for review by
management on a monthly basis, with certain levels being reviewed on a weekly basis.
e. An account balance is delinquent when a payment in full has not been received within forty-five (45) days
after receipt of first bill. An approved payment plan or loan is delinquent when a monthly payment is not
issued and remains unpaid thirty (30) days after the due date.
1. Credit Balance Accounts
a. FHH/FHMG will not refund insurance over-payments to the guarantor (patient or guardian) until all
accounts for which the guarantor is responsible are paid in full. "Paid in full" means that the total
account balance(s) owed are zero and not waiting for an insurance payment.
b. Approved refunds will be issued on a reasonable and regular basis.
2. Accounts Receivable
a. Patient statements, letters, or data mailers will be sent to patients on a 30-day cycle. Patients/guarantors
will receive four (4) or more statements within 120 days of the date on which the patient's financial
PROCEDURE:
Self Pay Collections, FN 101. Retrieved 04/2021. Official copy at http://fmh.policystat.com/policy/6960786/. Copyright ©
2021 Frederick Health
Page 2 of 5
COPY
responsibility has been determined.
b. Depending on the patient's balance, age of account, and other variables, phone calls may be placed with
patients/guarantors to collect on outstanding balances.
c. If the patient/guarantor has not made a payment within 120 days of the first billing date, or if the terms of
an approved payment plan are not being met, the account shall be eligible for placement with a collection
agency.
d. If a statement is returned to FHH/FHMG from the U.S. Post Office with an incorrect address, the account
will be researched to find a correct address. If a correct address is not found, the account shall be placed
with a collection agency prior to 120 days of the first billing date to assist in further collection efforts.
e. FHH/FHMG contact information and a notice of availability of financial assistance shall be included on all
statements or other communications regarding collection that are sent to the guarantor/patient.
1. Write-Off Review
a. If a patient account reaches a pre-determined aging with no account payment activity, or where the
terms of an approved payment plan are not being met, the account will be assessed for possible
small balance, bad debt or charity write off as follows:
i. Small Balance Write-Offs: An automated process will be used to identify accounts with a debit
balance. The accounts are processed with adjustment transactions and do not pass to bad debt,
but rather to established "small balance write-off" codes for balances outlined in the
Responsibility section of this policy.
ii. Bad Debt Write-Offs: A periodic report will be generated to "pre-list" self-pay and self-pay after
insurance accounts that may meet bad debt criteria outlined in the Responsibility section. Those
accounts will be subject to review by management, including based upon dollar balance, prior to
submitting into bad debt status.
A. Only specific employees in the PFS Department will be given access to the bad debt
functions in the patient accounting system.
B. Unless an administrative hold is placed on an account that has qualified for the bad debt
pre-list, all accounts will be moved into a bad debt status during the overnight batch
processing within the patient accounting system.
C. Consistent with Maryland law regarding balance billing, accounts with a third-party
insurance balance that have no insurance payment from the insurer for sixty (60) days may
have that balance deemed to be self-pay. At that time, the patient may begin to receive
statements in the same manner as a self-pay patient.
D. Wherever appropriate, write-offs shall be identified as charity care in accordance with FHH/
FHMG's Financial Assistance Policy. Any write-offs so identified will not be referred to any
outside collection agencies.
E. Patients may request, or may be requested by FHH/FHMG, to apply for Medical Assistance
(i.e., Medicaid) prior to being awarded financial assistance. This request may be made
prior to service, at the time of service, or during the billing and collection cycle. The account
in question will not be forwarded to a collection agency during the Medical Assistance
application process.
2. Debt Collections
a. Where appropriate, FHH/FHMG may use a bad debt collection agency to continue to try to collect on
Self Pay Collections, FN 101. Retrieved 04/2021. Official copy at http://fmh.policystat.com/policy/6960786/. Copyright ©
2021 Frederick Health
Page 3 of 5
COPY
greater than 120 day after first bill aged accounts (i.e., FHH/FHMG will not refer accounts to a collection
agency prior to 120 days after the first post-discharge billing statement). Patients with balances that have
been referred to a collection agency must resolve unpaid balances, request a payment plan, dispute
amounts owed or request financial assistance. Collection agencies may assess finance charges and fees
on the unpaid principal account balance to the extent permitted by applicable law and this policy.
b. For self-pay accounts that have not been assessed for financial assistance eligibility, FHH/FHMG shall
provide written notice to the patient or responsible party at least thirty (30) days prior to referring an
account to a bad debt collection agency. Such written notice shall:
i. Inform the patient of the availability of financial assistance;
ii. Identify the collection actions that FHH/FHMG plans to initiate to obtain payment;
iii. State a deadline after which such collection actions may be initiated that is no earlier than 30 days
after the date that the written notice is provided; and
iv. Include a plain language summary of FHH/FHMG's Financial Assistance Policy.
c. FHH/FHMG shall make a reasonable effort to orally notify the individual about FHH/FHMG's Financial
Assistance Policy and the process for applying.
d. Balances that remain open due to insurance denials will not be placed with a collection agency. However,
a collection agency may perform payer collections on insurance denials acting as an extension of the
business office.
e. Circumstances, such as pending eligibility for financial assistance or insurance coverage with Medicaid,
may delay an account from being referred to a collection agency.
f. Patients may file a grievance with FHH/FHMG regarding treatment or undesirable activities performed by
FHH/FHMG or contracted collection agencies regarding the handling of a patient's bill by contacting the
PFS Department. Any collection agency used by FHH/FHMG shall be instructed to forward to FHH/FHMG
any patient grievance filed with such collection agency.
g. FHH/FHMG shall not charge interest on bills incurred by self-pay patients before a court judgement is
obtained or engage in the following extraordinary collection actions ("ECAs") against an individual to
obtain payment for care: (i) selling an individual's debt to another party; (ii) deferring or denying or
requiring a payment before providing medically necessary care because of nonpayment of one or more
bills for previously provided care covered under the Financial Assistance Policy; (iii) forcing the sale or
foreclosure on an individual's real property; (iv) garnishing an individual's wages; (v) attaching or seizing
an individual's bank account or any other personal property; (vi) causing an individual's arrest; or (vii)
causing an individual to be subject to a writ of body attachment.
h. Although FHH/FHMG does not typically take such actions in the normal course of collection, it reserves
the right to pursue collections through the following ECAs at the direction of senior management after
verification of the individual's ability to pay: (i) reporting adverse information about an individual to
consumer credit reporting agencies or credit bureaus; (ii) placing a lien on an individual's property to
maintain its position as a secured creditor with respect to other creditors to whom the individual may owe
a debt; and (iii) commencing a civil action against an individual.
i. FHH/FHMG shall report the fulfillment of an individual's payment obligation within sixty (60) days after the
obligation is fulfilled to any consumer reporting agency to which it had reported adverse information about
the individual.
1. Financial Assistance
Self Pay Collections, FN 101. Retrieved 04/2021. Official copy at http://fmh.policystat.com/policy/6960786/. Copyright ©
2021 Frederick Health
Page 4 of 5
COPY
a. As a tax-exempt, not-for-profit hospital and medical group, FHH and FHMG are committed to providing
medically necessary care to patients in need regardless of race, sex, age, color, national origin, creed,
marital status, sexual orientation, gender identify, disability or ability to pay.
b. The Financial Counseling Team will be responsible for reviewing financial assistance applications and
appropriate related documentation and for determining eligibility based on FHH/FHMG policy guidelines.
c. Uninsured patients or those unable to pay in full for services rendered must contact FHH/FHMG's
Financial Counseling Team. The counselor will assist the patient and/or family in determining if he/she
qualifies for financial assistance. Cooperation is a necessary and integral part of the determination
process. Patients also may be eligible for financial assistance on a presumptive basis as further set forth
in the FHH/FHMG Financial Assistance Policy.
d. FHH/FHMG shall provide for a refund of amounts collected from a patient or guarantor who was later
found to be eligible for free or reduced-cost care on the date of service as described in the FHH/FHMG
Financial Assistance Policy.
e. If a patient is found to be eligible for financial assistance after FHH/FHMG has initiated ECAs, FHH/
FHMG will not take any further ECA and will take all reasonable steps available to reverse any ECA
already taken, as further set forth in the Financial Assistance Policy.
f. Patients may request FHH/FHMG to reconsider the denial of free or reduced-cost care as further set forth
in the Financial Assistance Policy.
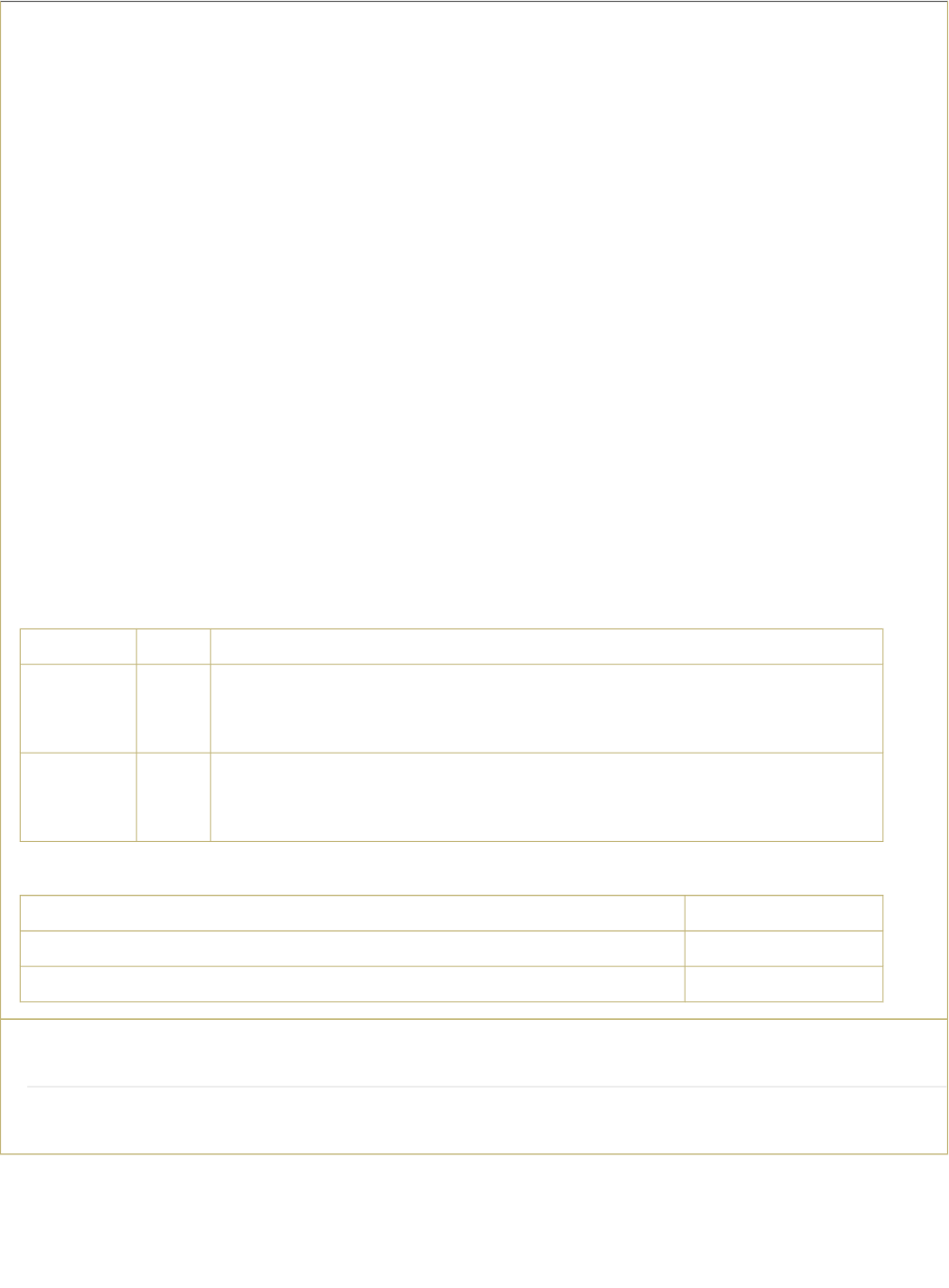
1. Responsibility
Criteria Other Criteria
Hospital >$10 Greater than 120 days from first post-discharge statement or 30 days after
written notice of intent to initiate collection actions, whichever is later. Action
must be reviewed by management prior to sending.
FHMG/
Professional
Service
>$5 Greater than 120 days from first post-discharge statement or 30 days after
written notice of intent to initiate collection actions, whichever is later. Action
must be reviewed by management prior to sending.
Criteria
Hospital $9.99
FHMG/ Professional Service $4.99
Attachments
No Attachments
Bad debt "pre-list" criteria used prior to bad debt placement:
Small Balance Criteria:
Self Pay Collections, FN 101. Retrieved 04/2021. Official copy at http://fmh.policystat.com/policy/6960786/. Copyright ©
2021 Frederick Health
Page 5 of 5
